Mapping the Mental Health Crisis
1 in 5 Americans is struggling with mental health, but care isn’t equally accessible to those who need it most, particularly in America's prisons
FORWARD THIS EMAIL — Send to a friend or read it as a web page
Interesting on the web
💊 Overdose deaths plummet more than 10%, saving thousands of lives - LINK
📲 Gen-Z hates social media, with some interesting demographic breakouts - LINK
📉 📈 Trump’s economy vs. Biden’s economy in 17 charts - LINK
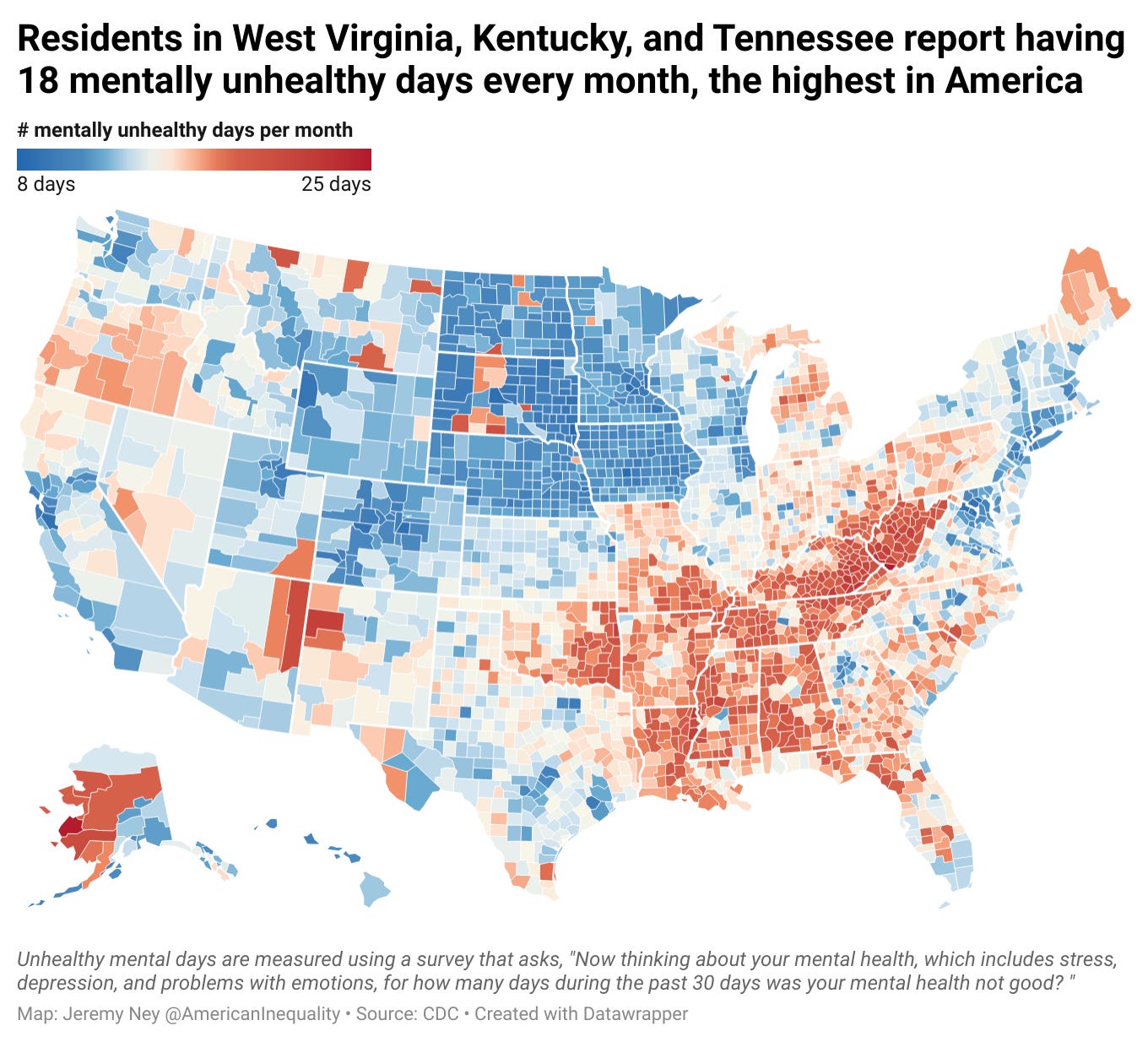
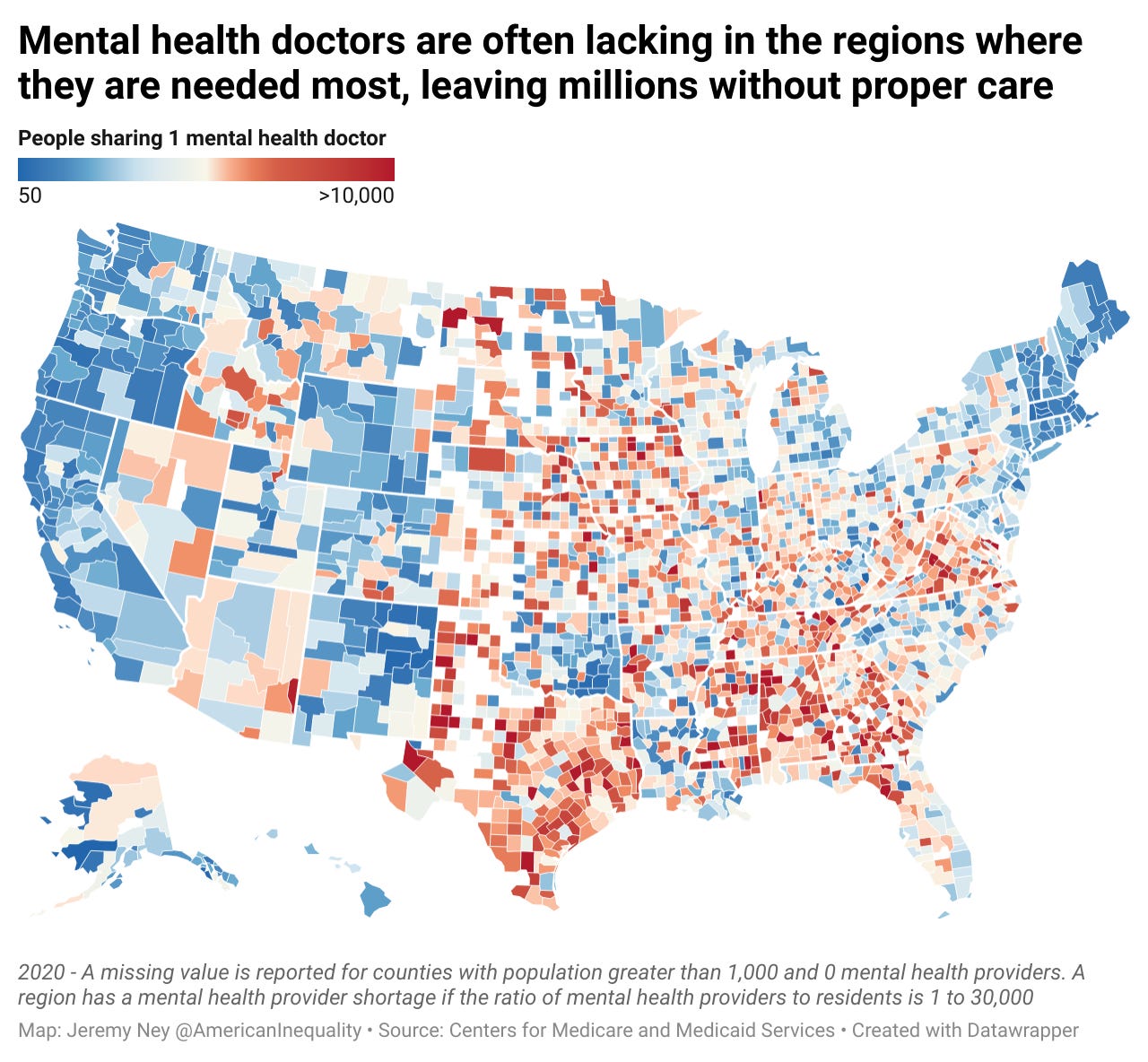
Mental health providers are not located where people are struggling with mental health. 1 in 5 adults in America is struggling with mental health and 43,000 Americans with an underlying mental illness die by suicide each year. However, mental health clinics and doctors are showing up in cities that have the most funds, rather than positioning themselves in the South and Mid-East where care is most needed.
New data is now available that helps us shed light on which regions in America are suffering the most with mental health challenges so we can focus our efforts here to help turn the tide. But even when facilities are located where we need them, stigma still dominates the conversation.
Tega Orhorhoro knows how difficult it is to talk about mental health. Growing up in New Mexico, her family struggled to address and understand her mental health:
“Growing up, mental health was not something that was talked about in my family. We would say that anxiety was a myth, depression was a myth and praying was the answer to all the problems. I would never bring up depression or my mental health because I felt like all I had to do was go to school and get good grades. So when I couldn’t eat or sleep from anxiety, I didn’t know how to articulate how I felt.”
When care isn’t provided in communities that need it most, people like Tega are left alone, struggling to find help.
Two datasets are instrumental in figuring out where policymakers, health advocates, and community organizations can focus their efforts to help Americans most in need. First, the CDC surveys Americans annually about their mental health (“Now thinking about your mental health, which includes stress, depression, and problems with emotions, for how many days in the past 30 days was your mental health not good?”) and second, the Center for Medicaid and Medicare Services keeps identifier records on the number of mental health providers in each county. This data helps us understand which regions in the US have the greatest strife as well as the least support.
Kentucky, Tennessee, and West Virginia have the highest rates of mental health challenges. Residents in these 3 states report on having 18+ mentally unhealthy days per month on average.

Residents in Massachusetts, on the other hand, report having the lowest number of mentally unhealthy days on a population weighted basis at 12.1 days. Massachusetts also has the best ratio of mental health providers to its overall population - There is at least 1 psychiatrist, psychologist, licensed clinical social workers, counselor, or specialized nurse practitioner for every 159 residents.
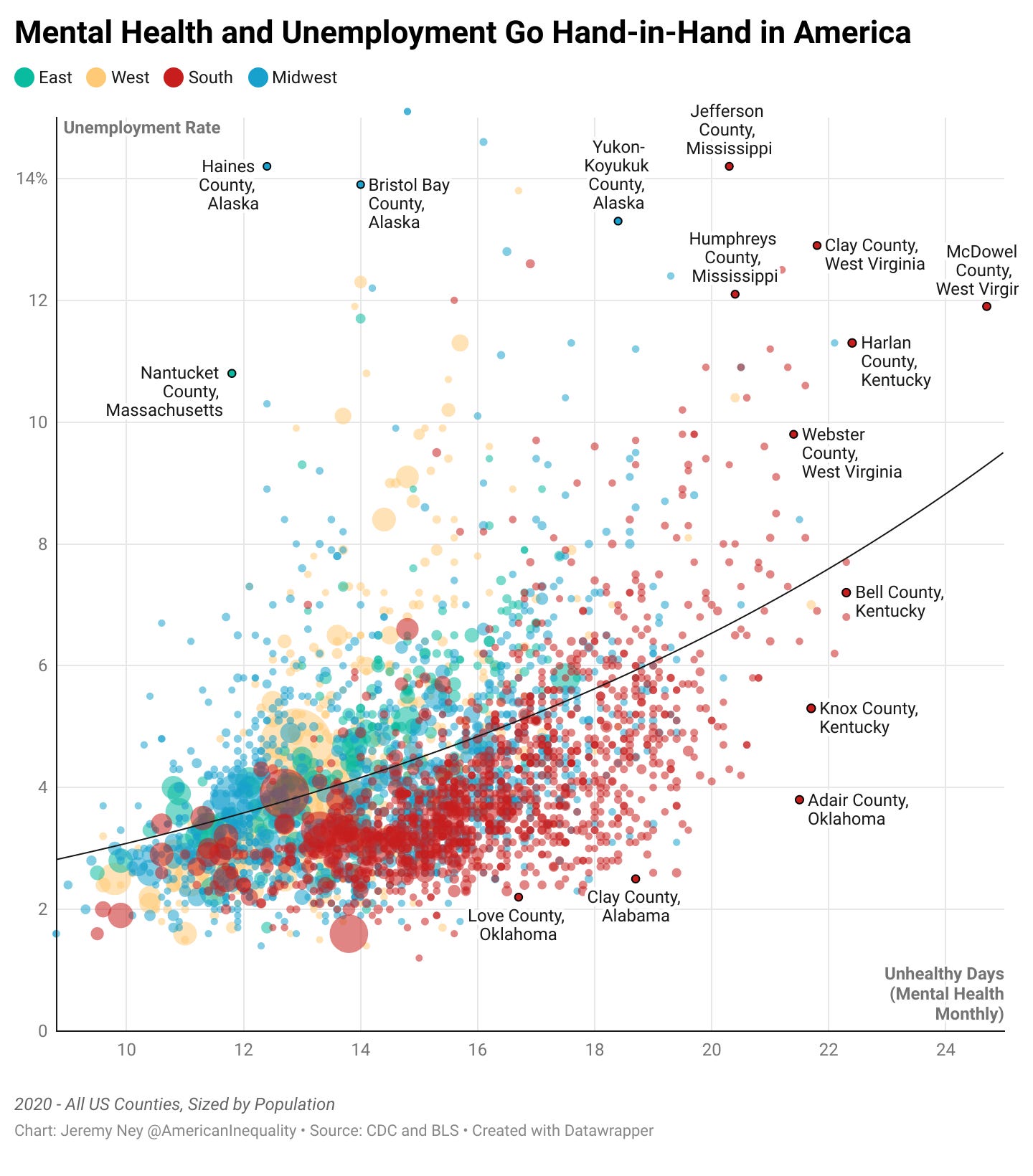
Mental health is deeply connected to unemployment, opioids
The chart above highlights the increasingly strong relationship between mental health and unemployment. The correlation between unemployment and mental health is highest when we look at southern counties alone. At the top of the chart, Jefferson County, Mississippi has an unemployment rate of 14%, while residents here report 21 mentally unhealthy days per month. CDC research shows that odds of depression are 3 times higher for unemployed than employed adults. Mental health and unemployment can also create a vicious cycle where those struggling with mental health may find it more difficult to get jobs due to stigma or lack of awareness, while a lack of a job may contribute to exacerbating mental health challenges like anxiety or depression.
The Boca Health Center provides key insights on how mental health challenges are interwoven with other issues like drug addiction. Depression and addiction commonly co-occur, and each condition can complicate the other. They show that 40% of people with depression also struggle with addiction.
Without mental health support, many are thrown in jail
McDowell, like many counties in America, has no resources for support. McDowell is one of 50 counties in America where every 10,000 residents has access to just 1 mental health provider. The Substance Abuse and Mental Health Services Administration (SAMSA) estimates that the US has a shortfall of 58,000 psychologists; 49,000 social workers; 27,000 mental health counselors, and 15,000 psychiatrists, not to mention the 78,000 school counselors that America needs.
Overall, 115 million people in the United States live in an area that is designated as a Mental Health Professional Shortage Area (HPSA), according to the Department of Health and Human Services. A region is deemed an HPSA if the ratio to mental health professional to residents is smaller than 1 per 30,000 people.
A mental health provider, by the definition above, is a psychiatrist, psychologist, licensed clinical social workers, counselor, marriage or family therapist, or mental health provider that treats alcohol and other drug abuse, as well as advanced practice nurses specializing in mental health care.
Dr. Kathy Pike, Professor of Psychology at Columbia University and CEO of One Mind , shared with us, “Even in the best served communities, there are not enough providers anywhere. The real issue is that there is more need everywhere.”
Despite this tremendous gap, the healthcare system overall has ways of adapting. Family medicine, internal medicine, psychiatry, neurology, and pediatrics have increasingly trained doctors to provide regular care for patients with mental health disorders. Just because a region lacks a psychiatrist or psychologist does not mean that it is completely without care. Still, 84 million Americans live in areas deemed primary care HPSAs.
Major cities tend to have the most providers. Los Angeles’s county has 34,521 mental health providers (with a ratio of 1 to 293 residents), Chicago’s county has 14,046 (with a ratio of 1 to 396) and Manhattan’s county has 13,986 providers (with a ratio of 1 to 116 residents).
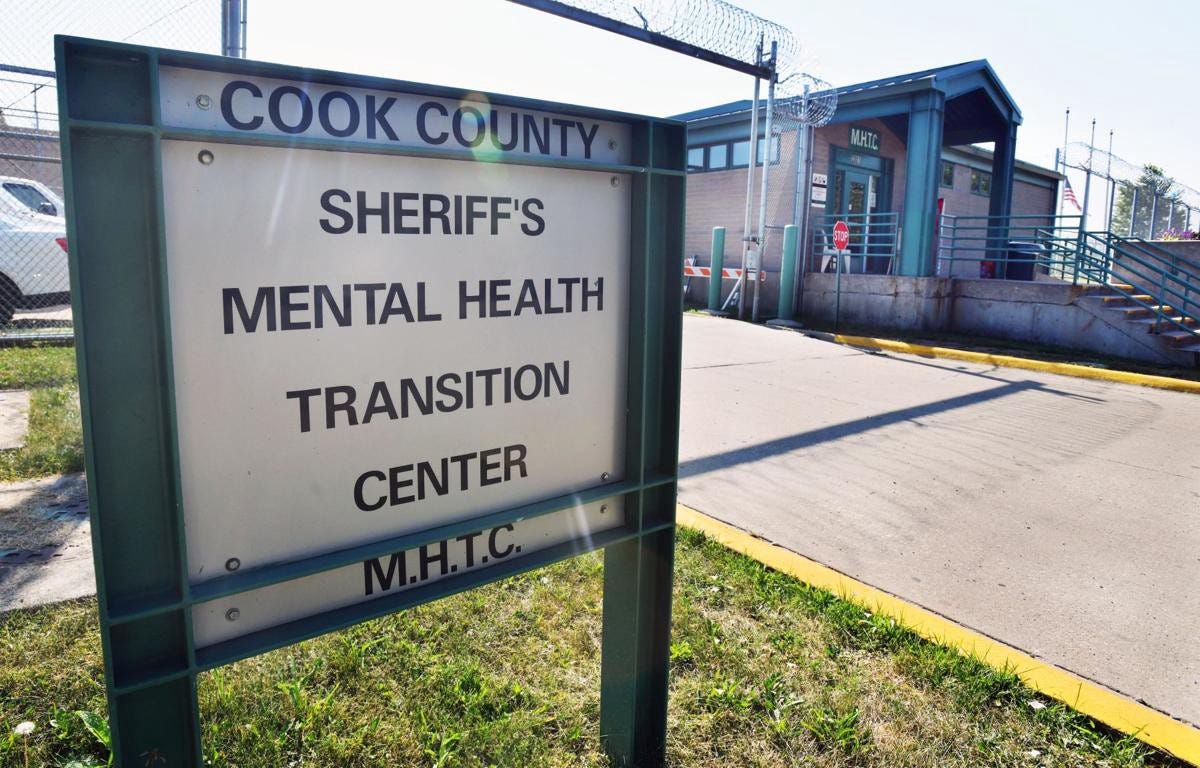
Instead, the three largest mental-health providers in the nation today are jails: Cook County in Illinois, Los Angeles County and Riker’s Island in New York. At least 400,000 inmates currently behind bars in the United States suffer from some type of mental illness — a population larger than the cities of Cleveland, New Orleans, or St. Louis — according to the National Alliance on Mental Illness. NAMI estimates that between 25-40% of all mentally ill Americans will be jailed or incarcerated at some point in their lives. All 3 prisons have been under federal investigation for officers beating and abusing mentally ill inmates.
The Path Forward
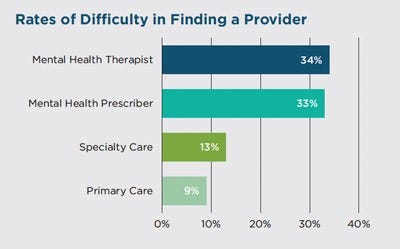
Stigma, diagnosis, and awareness are among the several reasons that mental health providers may not be located where mental health need is greatest. Only 43% of people with anxiety are actually being treated for it. In turn, millions of Americans suffer in school, lose their jobs, or lose their homes, thereby exacerbating already growing inequalities. The less we are able to help those in need, the further behind those families will fall.
💸 Re-orient Funding for Mental Health Block Grants — The Biden Administration is currently providing $825 million in Community Mental Health Services Block Grant funding to states and territories. These block grants allow states to determine how best to use their funds to combat growing mental health catastrophes. While funding has largely tracked population size (i.e. states get $0.35-$0.45 per person), funding could instead be calculated based on current need. Tennessee and Indiana roughly have the same populations and get roughly the same amount of funding, but Tennessee residents struggle with mental health at a rate 10% higher. In addition, the block grants could come with stronger accountability mechanisms, so America doesn’t see the same pitfalls that it felt in the mid-1980s.
👩🏫 Equip Schools with Better Mental Health Services — Half of all chronic mental illnesses begin by the age of 14, and yet we spend years before and after doing nothing to help people in need. We can improve interventions in schools to help young people before tremendous harm may emerge. Both Michigan and Arkansas provide strong examples here. Michigan developed a school mental health Medicaid service standard that provides psychological testing, counseling, case management, and social work services under the Individuals with Disabilities and Education Act, and provides a definition of the service and professional credentials for service provision. Arkansas developed a state policy and procedures manual, as well as procedures to approve school-based mental health programs within Arkansas public school districts. We cannot add this as another job for teachers, we need to help schools get the services they need to succeed.
Lessons from JFK
The last piece of legislation that John F. Kennedy signed before he died was the Community Mental Health Act. Kennedy’s vision was bold for the time: “We must move from the outmoded use of distant custodial institutions to the concept of community-centered agencies.” He wanted to replace asylums with community-based mental health centers that could provide “a coordinated range of timely diagnostic, health, educational, training, rehabilitation, employment, welfare, and legal protection services.”
Let’s return to Kennedy’s dream— let’s invest in services to care for those struggling with mental illnesses; let’s stop throwing people in jail when we don’t know how to address their challenges; and let’s send support to the regions in America that need it most.


An important topic. My daughter is a therapist and I know how important mental health professionals are. I could not find a therapist when I really needed one after my sister died unexpectedly. I was on multiple waiting lists. I think I got a call back about a year later, when I was better able to cope. I sure could have used some professional help in the earlier days.
Super interesting—
That map that you shared shows all of the Southern US states as exhibiting poor mental health. This is also where diets are rich in fried foods and coca cola, and lifestyles are terribly lacking exercise.
As a Midwesterner who moved to the South, the culture is eye-opening