Diabetes is Attacking My Family, We’re Not Alone
Tackling Systemic Inequalities for a Healthier Future: Guest Post
Yasmin Serrato-Munoz is the guest author for today’s article.
INTERESTING ON THE WEB
🪖 The military is now training army commanders on data literacy and data visualization - War on the Rocks
🤷♂️ In our last article we recommended raising wages for fast food workers to help lower poverty. California enacted that law this week, and in turn McDonalds, Chipotle, and other raised their food prices - CNBC
🗺️ An extremely detailed map of NYC and great way to check your New York knowledge - The Upshot
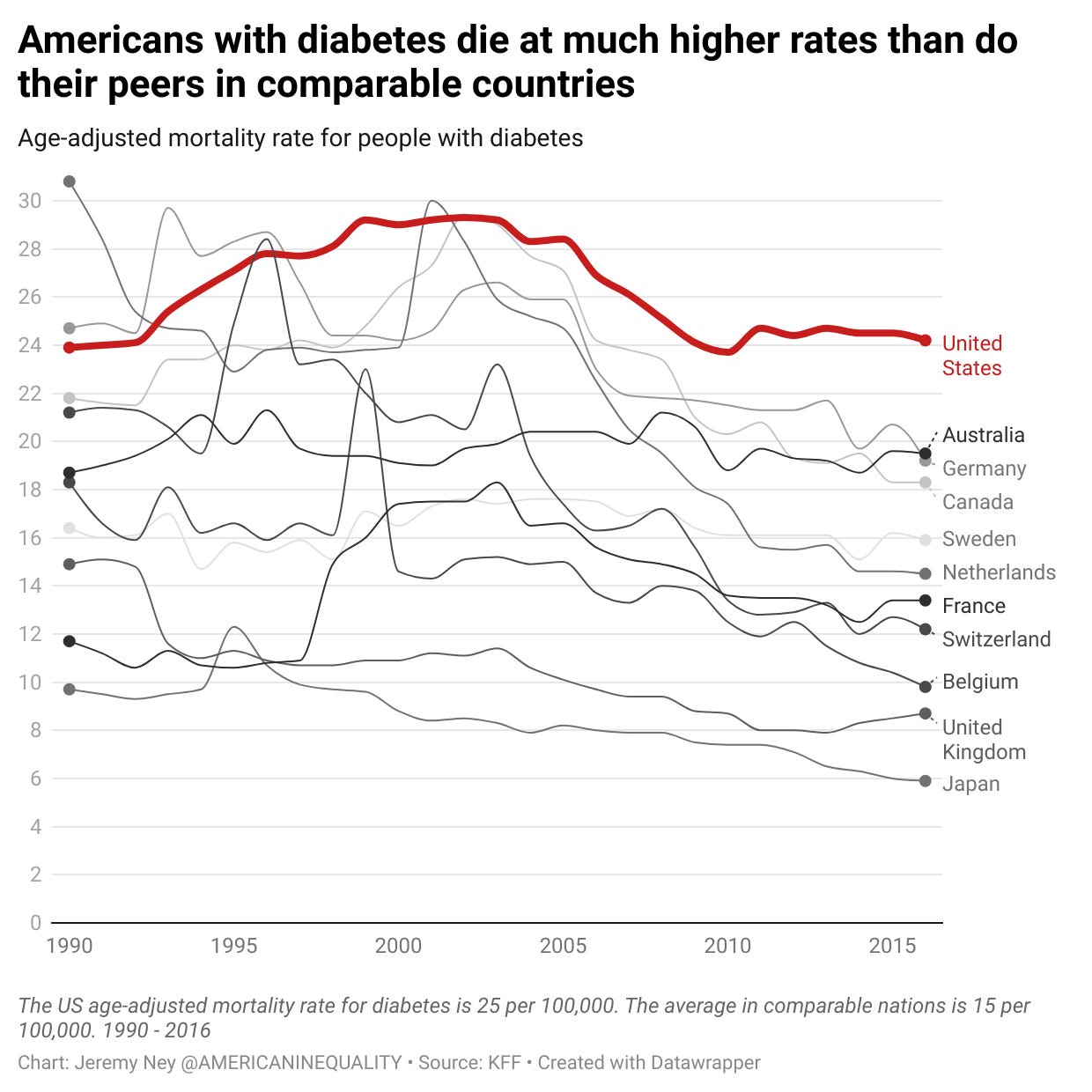
My grandmother is dying from diabetes, along with 37 million other Americans. In 2021, diabetes killed 103,294 people, making it the 8th leading cause of death. Behind those numbers is a more complex story that shows the true shape of healthcare, inequality, and opportunity in America.
A type 2 diabetes diagnosis at the age of 30 can reduce your life expectancy by 14 years.
As more drugs come to market like Ozempic, Mounjaro, and Zepbound, which the FDA just approved on November 8, more Americans are trying to figure out how to successfully navigate their diabetes and overall health. However, the high prices of these drugs (Zepound is $1,060 per month) and uncertainty about who should take them may still lead to certain inequalities.
Diabetes, the Hidden Killer
For every decade earlier that a person develops diabetes, that individual loses 3-4 years of life expectancy. Developing type 2 diabetes at age 50 can decrease a person’s life expectancy by 6 years.
According to the CDC, of those 37 million Americans with diabetes, one in five do not know they have the disease. This is often due to poor access to care in rural areas or because doctors are more likely to misdiagnose or turn away Black and Hispanic patients.
After my grandmother’s health took a turn for the worse, my mother realized that many of her own symptoms were similar. After several visits to the doctor, she too was diagnosed with diabetes. The CDC acknowledges that having a parent with diabetes means that children are more likely to have it too. Many of the doctors she saw did not listen to her questions, and instead just prescribed her medicine. Her frustration was met with determination. As she started educating herself about diabetes and nutrition, she became more physically active.

The lifesaving measures required to treat and manage diabetes are not cheap. About $1 out of every $4 dollars spent in the US healthcare system is spent treating someone with diabetes. According to the CDC, diabetes costs the healthcare system $237 billion dollars in direct medical costs and $90 billion in reduced productivity. These costs may be understated as diabetes often comes with complications such as heart disease, fatty liver, and increased risk of stroke. Medicare recipients over the age of 65 and living with Type 2 diabetes can expect to pay $5,876 per year out of pocket.
While insulin prices are capped at $35 for those with Medicare, an insulin pen can range from $60-$140 without insurance. Millions of Americans need daily insulin shots or require multiple doctor’s visits per month. For those without adequate healthcare coverage or insurance (who are disproportionately those living in poor rural areas or people of color), this cost can be the most painful.
Popular medications like Ozempic, which not only treats diabetes but also aids weight loss, can cost more than $1,000 a month. Low income individuals cannot keep up with the costs of their medications, resulting in complications and additional costs.
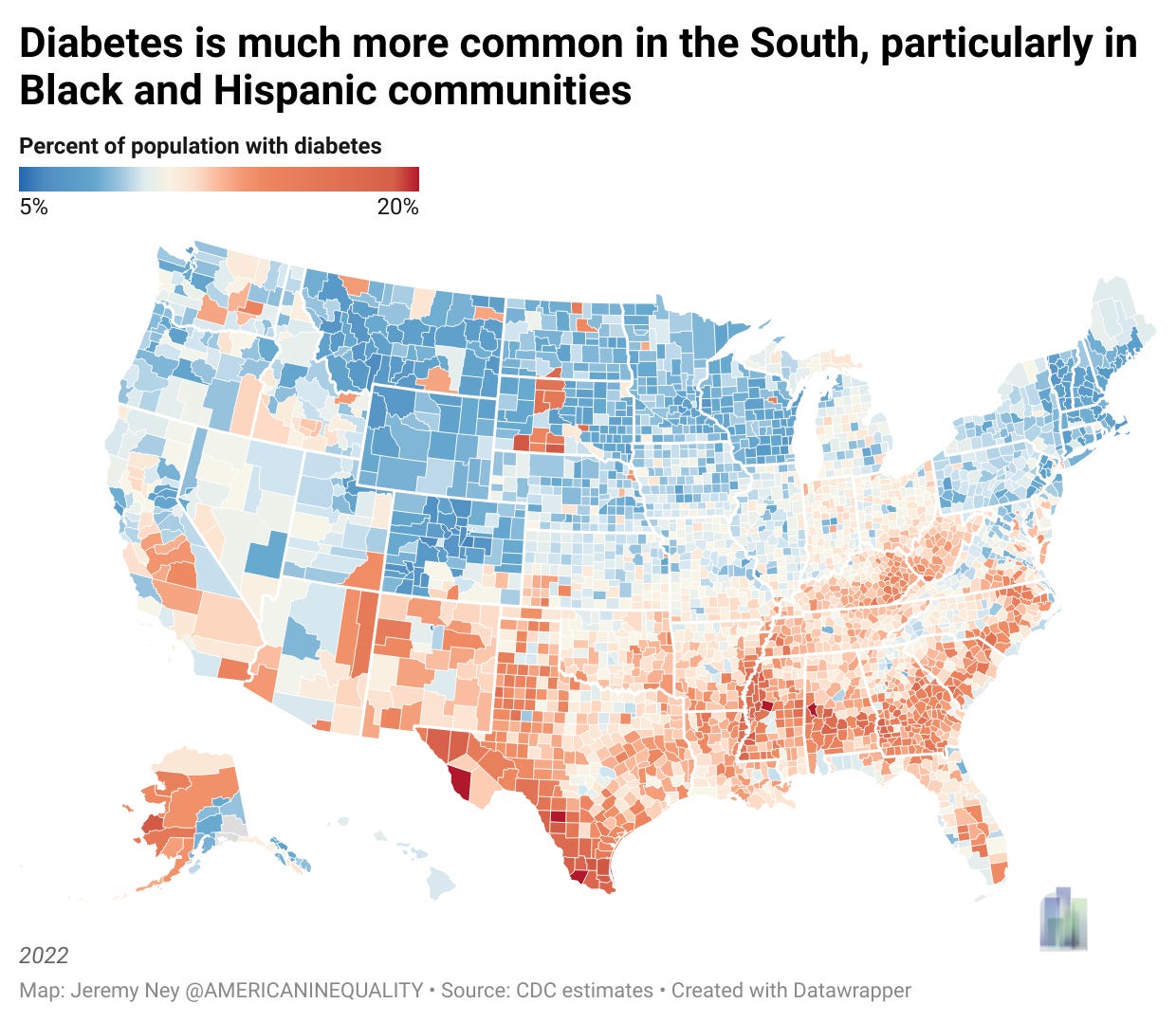
The southern border of Texas and the Mississippi Delta are the regions that are struggling most with diabetes. In Starr County, Texas in 1 in 5 residents lives with diabetes, though the number is likely far higher. We had previously spotlighted Starr County, Texas in another one of our posts, since Starr County is the least English-speaking county in America. One in two residents lacks proficiency in English. One in three people there live in poverty – the median income is $31,000 and the population is 66,000.
Children in Poverty are at Much Higher Risk of Diabetes
Children living in poverty often lack adequate nutrition, and in turn have a higher predisposition towards developing diabetes than children who live above the poverty line. In our analysis, we found a 79% correlation between child poverty rates and diabetes rates.
Once impoverished children develop diabetes, they are much less likely to receive the care they need. Children in poverty also visit the doctor far less than their wealthier peers and get worse care when they do. A doctor’s visit requires a parent/guardian to take time off from work and unfortunately that is often not an option for some families. Without doctor’s visits, children’s healthcare is left up to chance. The chance that hopefully everyone is healthy.
In my family, we used to refer to this as “God’s healthcare plan” - pray you don’t get sick because we can’t afford it.
The lack of nutritious food available to children living in poverty fuels this relationship to diabetes. Children living in poverty often live in food deserts and have to rely on fast food chains or convenience stores. These tend to lead to childhood obesity. Children and adolescents in the lowest income bracket had an obesity prevalence of 18.9% while those in the highest income bracket had an obesity prevalence of 10.9%. Being overweight during childhood increases the risk of obesity in adulthood, and in turn the risk of diabetes. 1 in 4 Black children is obese compared to 1 in 6 White children.
Racial Divides Lead to Lower Life Expectancies
Diabetes is one of the most lethal diseases in America for people of color. Black Americans are 2.5 times more likely to be hospitalized from diabetes complications and twice as likely to die from diabetes as White Americans. Hispanic Americans are 70% more likely to be diagnosed with diabetes and 1.3 times more likely to die from diabetes as White Americans. Diabetes complications combined with poor access to healthcare, can create a fatal combination.
Tracking diabetes rates over the last twenty years, we see diabetes rates increase for all ethnicities. However, the rates of Black and Hispanic Americans are almost twice that of White Americans. In order to decrease diabetes prevalence and decrease death rates, a few systemic inequalities must be addressed.
The Path Forward
Doctors and the private sector are most responsible for addressing diabetes and inequality. If we want to create solutions, we need to focus on prevention, detection, and thoughtful action.
🍔 🥗 Improve in low-income communities: One of the biggest drivers of diabetes is poor nutrition: sugary sodas, sweet snacks, and fast foods. In food deserts, Black neighborhoods, and in low-income communities these food types are much more available. Several studies have shown that neighborhoods that increase access to healthy food options by establishing community gardens, food pantries, and changing school cafeteria menus saw a meaningful decrease in community diabetes rates for children. One study in California showed that this decreased diabetes rates by 23%.
🕵️♂️ Increase diabetes detection rates: 1 in 5 Americans doesn’t know they have diabetes. This occurs because either the patient didn’t visit the doctor or were misdiagnosed by a doctor when they did visit. Mobile clinics can reach communities, particularly rural, Black, or low-income communities that often fail to get healthcare access. In Ruston, Louisiana, the Health Hut mobile clinic helped diabetic patients see a 20% decrease of glycated hemoglobin (HbA1c) levels.
🤝 Address medical cultural competency: Even if doctors can reach these patients, we need to ensure medical professionals properly diagnose and treat patients for diabetes. Medical professionals may not be aware of cultural norms or speak the language of their patients, and which can create divides for patient care. Several studies show that improving cultural competency has led to higher rates of patient check-ins for diabetes and improved likelihood of telling neighbors to visit the doctor as well. Medical providers should be trained on cultural norms of the population they serve. Having a medical staff that speaks different languages will help patients feel comfortable.
Diabetes rates are likely to continue to rise without early prevention, detection, and access to healthcare. Systemic inequalities like poverty, the built environment, and lack of resources exacerbate the challenges that contribute to Black and Hispanic communities having diabetes at higher rates than do their wealthier and white counterparts.







Hugely important topic and startling to see those numbers on the impact for life expectancy