Without health insurance, poverty is just a medical bill away
Remember the Affordable Care Act? We still have a long way to go
American Inequality has now hit +7,000 email subscribers! 🎉 Send to a friend and tell them to join our rapidly growing community 🚀
INTERESTING ON THE WEB
Great free class from On Data & Design on how to map out data - YouTube
Visualizing how Colorado River water gets used up (spoiler alert: the data viz is a river) - The New York Times
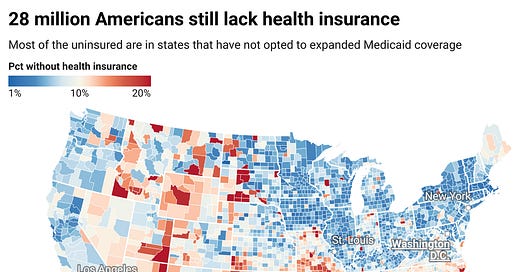
America is the only high-income country that does not guarantee health coverage for all its citizens. As a result, 28 million Americans still have no health insurance. In 2018, medical bills forced 8 million people into poverty. Despite the devastating effects of the COVID-19 pandemic over the last 3 years, insurance rates have not meaningfully changed. When we dig into specific states, Texas is a microcosm of the country’s broader issues, with the lowest health insurance coverage rates in the country, leading to massive inequality across communities.
Lack of health insurance produces inequalities. Families without insurance have higher child mortality rates than those with insurance and lower overall life expectancies. They are 20% less likely to seek the care they need, and they are 2x more likely to have trouble paying medical bills, causing cycles of poverty.
The Affordable Care Act (ACA), often referred to as Obamacare, made tremendous strides in reducing the share of uninsured Americans. Since 2010 when the ACA was passed, the number of uninsured Americans has fallen by nearly half, from 15.5% of the population to 8.3% of the population (48 million Americans to 28 million Americans). In the last year alone, a record-breaking 16.3 million people selected a healthcare option from the ACA open marketplace. Nevertheless, over the last 7 years the share of uninsured Americans have largely stagnated, which is why we thought this would be a great topic to cover.
High costs decrease insurance enrollment
The #1 reason Americans cite for not having insurance is the high cost of enrollment. Access is available, but costs keep people out. Although the ACA helped households save an average $800 annually on their annual premiums, the average annual premium for employer-sponsored health insurance is $7,739 per year for single coverage and $22,221 per year for family coverage.
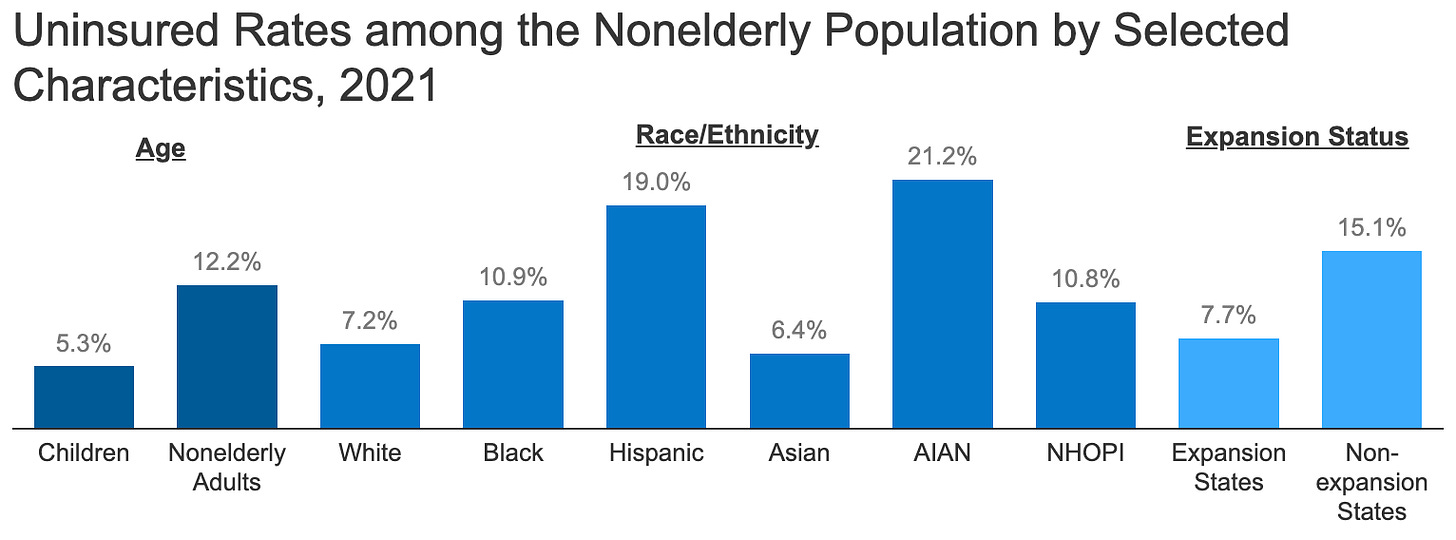
13 million of the 28 million uninsured Americans are in low-income households earning 200% below the federal poverty line. Elderly Americans are the least likely demographic to be insured, often because health insurance costs are much higher for this group than for younger, healthier adults. Nearly half of the uninsured population are people of color.
Texas has the lowest share of insured residents because it suffers from the perfect storm of healthcare challenges - poor state support, high costs, and systemic factors. Nearly 1 in 5 Texans does not have health insurance, more than double the national rate.
First, the state has not expanded Medicaid coverage, which has prevented 1.4 million families from otherwise getting health insurance. Many of these families are living in poverty. But 10 states have not expanded Medicaid as well, so what else makes Texas special?
The second arm of the perfect storm in Texas is that it has high healthcare costs. Texas is the 4th most expensive state for healthcare, with residents spending $17 out of every $100 on healthcare costs. There are fewer rules on how much doctors can charge for procedures and the state has fewer facilities, particularly in remote regions - all of which drive up costs. The impact of lost earnings and poor health in Texas is expected to rise from $57 billion in 2016 to $178.5 billion by 2040.
Finally, Texas’s large immigrant population has led to a lower share of the population receiving health insurance. Non-citizen immigrants are 3x more likely to lack insurance than are American citizens. Immigrants can be both less likely to get insurance because they are excluded from certain systems - perhaps they can’t get government issued ID cards or their jobs only recognize them as contractors - or they are excluded because high prices make insurance inaccessible.
What is Medicaid expansion?
‘Medicaid expansion’ is a major component of the Affordable Care Act, which stipulates that state can provide health insurance to residents who earn less than $18,754 (or $38,295 for a family of 4) by using federal funds to pay for that coverage. States are able offer this benefit because under the ACA the federal government agreed to reimburse states for 90% of the costs. In National Federation of Independent Business et al v. Sebelius, the Supreme Court ruled that states could not be coerced into expanding Medicaid.
Employer insurance distorts market forces
Half of Americans, or 156M people, get their insurance through their employer. An additional 60 million Americans are covered under Medicare, 58 million are covered under Medicaid, and 12 million are covered under military insurance.
Employer sponsored health insurance did not develop because the Founding Fathers wanted it this way. Instead, it grew because of war and taxes. During WW2, FDR signed Executive Order 9250 to prevent companies from raising wages too quickly as the American workforce went to fight overseas. Companies in turn started competing on benefits, namely by offering more generous health insurance. By 1943, the IRS determined that employer-based health insurance should be exempt from taxation, making it cheaper to get health insurance through a job than by other means. In 1940, only 9% of Americans had health insurance. Following the IRS’s changes, 50% had insurance by the end of 1950.
“Job-lock” occurs when employees stay in jobs they’d otherwise leave because they don’t want to lose their insurance. 1 in 3 employees in America say that they would leave their job if it didn’t also mean losing their insurance. This creates a perverse incentive in the market, with some researchers estimating that insurance based job-lock reduces employment mobility by 25%. The Congressional Budget Office has similarly calculated that 2.5 million Americans pick their jobs based on the insurance benefits offered.
For Kirk Eichenwald, “Health insurance rules my life.” Kirk has a pre-existing condition, like 133 million other Americans, which has not only created job-lock for him, it has also defined his choices in life. Kirk has had chronic seizures from epilepsy since he was 18, often ending up in the hospital. When he convulsed in public, strangers often called him an ambulance which he could hardly afford. While the ACA probably saved his life, he’s working on getting German or English citizenship to ensure he’ll be covered regardless of how the political winds blow.
As the field of gig-work grows, these employees continually struggle to find affordable insurance since their employers rarely provide this benefit. 23% of gig-workers lack insurance, despite the fact that many of them may be eligible to get care of coverage through the ACA for as little as $10 per month through multiple tax credits.
When millions of workers lost their jobs during the pandemic, Hispanic Americans and Asian Americans were most negatively impacted from losing their employer sponsored insurance.
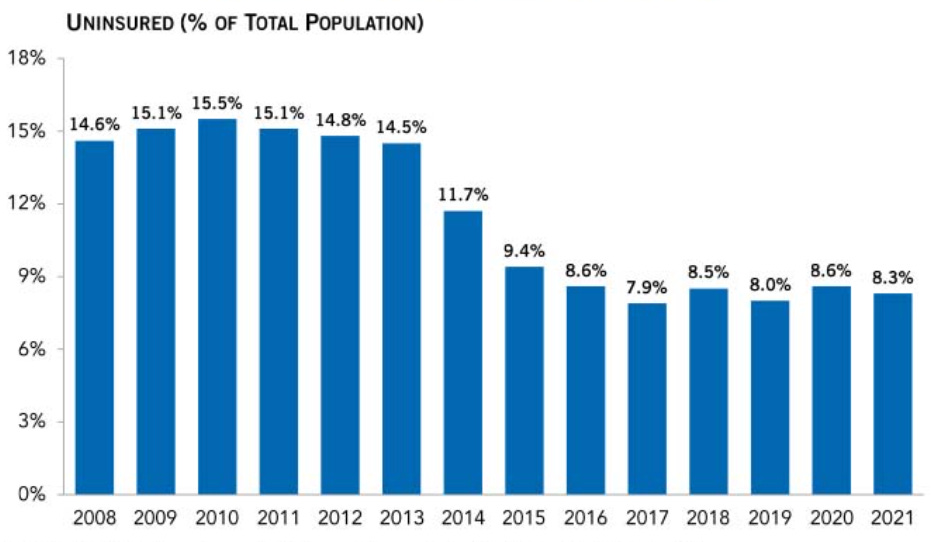
The insurance rate has largely stagnated as federal and state efforts to get Americans enrolled have slowed. While the Obama administration put a huge emphasis on increasing insurance enrollment from 2010 to 2016, the Trump administration made no similar effort. Although the Biden administration has renewed efforts, the data has not yielded new results.
The Path Forward
32 countries offer free healthcare to their citizens. America spends far more on health insurance, yet we live far shorter lives. On a national scale, the U.S. spent 17.8% of GDP on healthcare, nearly twice as much as the average OECD country. The dollars spent do not translate to the desired health benefits. While the US has a long way to go before ever reaching the model of those 32 countries, there are several lessons to learn from global communities.
🤝 Expand Medicaid coverage - As we’ve written about many times before, expanding Medicaid can help more than 2.1 million Americans receive affordable health insurance. Wyoming, Kansas, Texas, Wisconsin, Tennessee, Mississippi, Alabama, Georgia, South Carolina and Florida have yet to adopt the expansion of Medicaid, which directly hurts eligible low-income families who need health insurance. These states are leaving money on the table that can help increase coverage. With state revenues declining, particularly in the South, this comes at a crucial time. People living in Medicaid expansion states not only live longer, but a 2017 study found that they have “improved credit scores, reduced balances past due as a percent of total debt, reduced probability of a medical collection balance of $1,000 or more, … and a reduction in the probability of a new bankruptcy filing.”
👨⚕️Provide universal coverage - The “medicare for all debate” completely misses the point. Healthcare should be about providing a safeguard for the sick. How we implement that system, and who pays for it, are the secondary instruments. Dr. Aaron Carroll, the Chief Health Officer of Indiana University, spent years analyzing how 5 countries provide healthcare and I agree with his conclusion:
“Insurance is really just about moving money around. It’s the least important part of the health care system. Universal coverage matters. What doesn’t is how you provide that coverage, whether it’s a fully socialized National Health Service [like in Britain], modified single-payer schemes [like in Canada], regulated nonprofit insurance [like in Australia and New Zealand] or private health savings accounts [like in Singapore].”
✂️Simplify the system to avoid inequality pitfalls - America has far too many insurance schemes that prevent households from getting adequate coverage. COBRA. Veterans Affairs. Medicare. Medicaid. Obamacare Exchanges. Employer-based. Whether you are the entirely private healthcare system of Switzerland or the fully public National Health Service of the UK, America needs to reduce the complexities of the healthcare system to ensure people don’t get stuck in cycles of health insurance debt. 71% of all people disenrolled from Medicaid this year had their coverage terminated for procedural reasons, which is alarming because people who lose coverage for procedural or paperwork reasons may still qualify and be in dire need. Rachel Munsie has seen these pitfalls up close as the CEO & cofounder of Ounce, a company that partners with health insurers to provide care coordination and benefit enrollment to residents of affordable housing. Rachel shared with me:
“Most people would be shocked by the amount of complex paperwork and processes needed for a typical Medicaid recipient to stay covered each year. It gets even more complicated when someone is eligible for multiple plans at the same time. Health plans and government agencies operate in silos, but in an ideal world we could capture someone’s data in a single place and automatically verify eligibility in a simple and seamless way.”
When families lack reliable health insurance, inequality follows shortly afterwards. 1 in 10 Americans carry medical debt, and those who carry this debt are far less likely to seek help. Healthcare is deeply connected to opportunity, particularly because it’s so closely linked with employment. It’s time to break the stagnation in insurance enrollment and get more families the backstop they need.







Great article. I went without insurance for 8 years, post divorce, because I refused to pay high premiums for a high deductible plan. I crossed my fingers and prayed that nothing would happen. Thank goodness I’m now old enough for Medicare. I still hope nothing major happens.
Thanks for your thoughtful article, exposing these data more broadly might help promote change. I left the US with family more than 15 years ago to escape the 'pre-existing condition' issue which could at that time threaten a sick individual with death and their family with bankruptcy. The ACA, implemented in 2010 after we left, had beneficial outcomes but falls very short of the kind of healthcare coverage framework you argue for. (For information I am a resident of France.)
I'd quibble on two points: (1) It is flattering to call how healthcare is managed in the US a 'system', unless the binding element in calling it thus is 'capitalism.' (2) You write, "Healthcare should be about providing a safeguard for the sick." In many of the other 32 countries your article refers to it is not just about people who require treatment; it is also about proactivity in screening, testing and vaccinating to prevent sickness in the first place. There is, of course, an obvious link when discussing healthcare to regulatory matters, such as workplace safety and the gun violence epidemic in America.
Finally, my modest contribution to the debate is found here: https://leavingamerica.substack.com/p/it-doesnt-have-to-be-this-way-healthcare?r=1u1uw5